Symptoms before bronchiectasis hemoptysis
summary
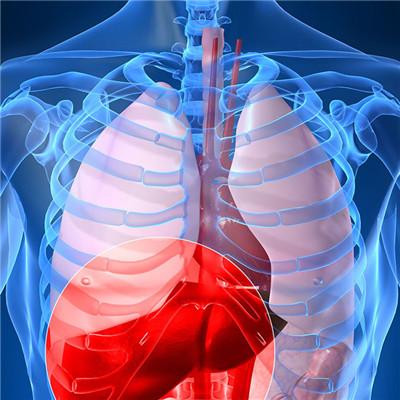
Bronchiectasis is mostly secondary to acute and chronic respiratory tract infection and bronchial obstruction. Most patients have childhood history of measles, pertussis or bronchopneumonia. The main clinical manifestations were chronic cough, cough with a lot of purulent sputum and (or) repeated hemoptysis. In recent years, with the appropriate treatment of acute and chronic respiratory infections, the incidence rate has decreased.
Symptoms before bronchiectasis hemoptysis
The main symptoms of bronchiectasis were chronic cough, cough with a lot of purulent sputum and repeated hemoptysis. Expectoration in the morning, evening and bedtime, up to 100 ~ 400ml per day, many patients in other times almost no cough. Patients feel relaxed when expectoration is unobstructed; If the sputum drainage is not smooth, the chest tightness and systemic symptoms will be aggravated.
Sputum is mostly yellow green pus like. When anaerobic bacteria are infected, it can be stinks. All day sputum is collected in glass bottles. After a few hours, the sputum can be divided into 3 layers: the upper layer is foam, the middle layer is yellow green turbid pus, and the lower layer is the necrotic tissue sediment. 90% of the patients often have hemoptysis, the degree of hemoptysis is not necessarily parallel to the severity of the disease, the scope of the disease.
In some patients, hemoptysis may be the first and only chief complaint, clinically known as "dry bronchiectasis", common in tuberculous bronchiectasis, lesions in the upper lobe of the bronchus. If repeated secondary infection, can appear systemic toxic blood symptoms, patients sometimes have fever, night sweats, fatigue, loss of appetite, emaciation and so on.
matters needing attention
"Track sign" and "ring sign" are typical imaging features of bronchiectasis, which are helpful to the clinical diagnosis of bronchiectasis. However, it is necessary to differentiate bronchiectasis from pulmonary cyst in clinic. In addition to the identification of history and symptoms, the key points of imaging identification were the thickness of the cyst wall, the size of the cyst cavity and the location of the lesion. The wall of pulmonary cyst is thin, there is no inflammatory exudation around, the cavity is large, and it mostly occurs in the middle and outer zone of lung. Bronchiectasis has small lumen, thick wall, inflammatory exudation around, and mostly occurs in the middle and inner lung zone.