How should chronic pericarditis treat?
summary
After acute pericarditis, scar adhesion and calcinosis can be left on the pericardium. Most patients with only slight scar formation and loose or local adhesion, pericardial no obvious thickening, does not affect the function of the heart, known as chronic adhesive pericarditis, has no clinical significance, some patients with pericardial effusion exists for a long time, the formation of chronic exudative pericarditis, may be the chronic process of acute nonspecific pericarditis, how should chronic pericarditis be treated?
How should chronic pericarditis treat?
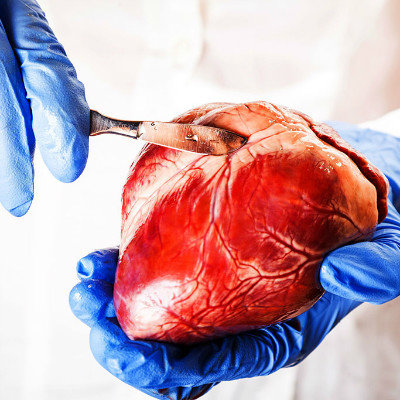
In the treatment of chronic pericarditis with western medicine, pericardial dissection should be performed as soon as possible. Long course of disease, myocardial atrophy and fibrosis often affect the effect of surgery. Therefore, as long as the clinical manifestation is progressive compression of the heart, which can not be explained by simple pericardial effusion, or the signs of heavy compression of the heart become more and more obvious during the absorption of pericardial effusion, or the mural pericardium thickening is found during pericardial cavity gas injection, or the pericardium thickening and narrowing are shown by magnetic resonance imaging, if the pericardial infection has been basically controlled, the operation should be carried out as soon as possible. Patients with tuberculous pericarditis should consider operation after the activity of tuberculosis has been static, so as to avoid the spread of tuberculosis caused by early operation.

Dyspnea after exertion is often the earliest symptom of constrictive pericarditis. It is due to the relatively fixed cardiac output, which can not be increased during activity. In the later stage, due to a large amount of pleural effusion, ascites will elevate the diaphragm and congest the lung, resulting in dyspnea at rest, even sitting breathing, a large number of ascites and swollen liver oppressing the abdominal organs, In addition, there may be fatigue, hypogastric appetite, dizziness, weakness, palpitation, cough, epigastric pain, edema, etc.
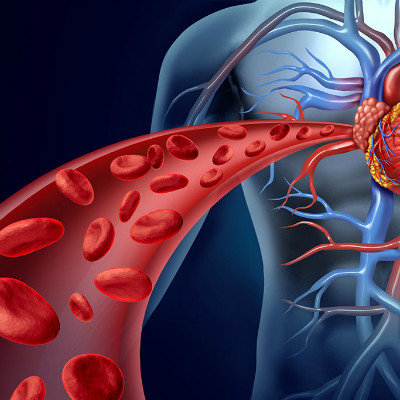
Manifestations of cardiac compression: jugular vein, liver swelling, ascites, pleural effusion, edema of the lower extremities, etc. * these are associated with cardiac diastolic obstruction, resulting in a decrease in cardiac output, resulting in renal retention of water and sodium, thereby increasing blood volume, and obstruction of venous return, which is associated with increased venous pressure. Different from general heart failure.
matters needing attention
Adjust daily life and workload, regular activities and exercise, avoid fatigue. Maintain emotional stability, avoid emotional excitement and tension. Keep defecation unobstructed, avoid forced defecation, eat more fruits and high fiber food. Avoid cold stimulation and keep warm.