Postpartum acute nephritis symptoms?
summary
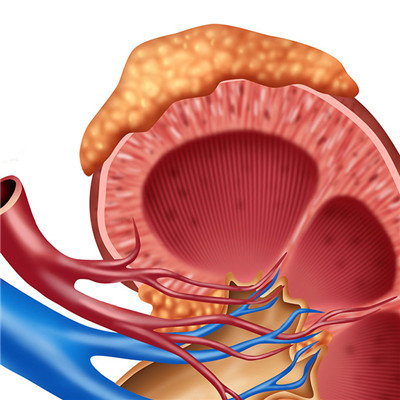
Postpartum acute nephritis is a common disease, patients with acute nephritis should be treated as soon as possible. What are the symptoms of acute nephritis? Next, let the experts to introduce to you, let you have a more comprehensive understanding of the symptoms of postpartum acute nephritis, hope to help you.
Postpartum acute nephritis symptoms?
1. Gross hematuria was found in 40% - 70% of the patients; Urine color, such as meat washing water sample or black tea and soy sauce sample, lasts for about 1-2 cycles, which is microscopic hematuria. Most of the hematuria disappeared within 6 months and lasted for 1-3 years. In the early stage of the disease, the urine volume was significantly reduced, even no urine (the urine volume of the whole day was less than 100 ml). If the urine volume was less than 3 days, it indicated that the disease was serious. At this time, azotemia often occurred (blood urea nitrogen > 7.14 mmol / L); It indicates that renal function is impaired. In the recovery period of the disease, the urine volume increased gradually, which could reach more than 2000 ml, and the renal function could gradually return to normal.
2. proteinuria acute glomerulonephritis patients almost all albuminuria, manifested as increased foam in the urine, usually increased with the severity of the disease, proteinuria is slower than other symptoms disappear, after the edema disappeared, proteinuria is still 1 to 2 months, or even longer will gradually subsided.
3. Edema is often the first symptom of onset, which is seen in 70% - 90% of cases. Light only for eyelid edema, serious can extend to the whole body, some patients will appear hydrothorax, ascites and other symptoms. Edema generally begins to subside within 2-3 weeks, and urine volume will gradually increase. 4. About 80% of patients with hypertensive acute glomerulonephritis may have hypertension. The blood pressure is usually increased to a moderate degree. In adults, it is generally 18.7-22.7kpa / 12.0-14.7kpa. Occasionally, more serious cases may develop into hypertensive crisis, but the diastolic blood pressure rarely exceeds 16kpa. If the blood pressure continues to rise, it is the precursor of chronic nephritis, indicating that the kidney disease is more serious. 5. General symptoms in addition to the above clinical manifestations, patients often have general discomfort, fatigue, low back pain, frequent urination, numbness and other symptoms. Some patients may have prodromal infection, such as sore throat, body heat, skin ulcer and other symptoms.
matters needing attention
1. The edema of chronic nephritis with high salt diet is closely related to blood volume and sodium salt, so we must limit salt and give low salt diet. The daily intake of salt should be controlled below 2-4G in order to prevent swelling and blood volume from increasing. 2. Patients with high-fat food nephritis generally have symptoms of hypertension and anemia. If there is a large amount of animal fat, it will have a great bad effect on hypertension and anemia. The main reason is that animal fat can aggravate arteriosclerosis and inhibit hematopoietic function, so patients with nephritis must be careful to eat. But nephritis without fat intake, the body will become more weak, so in daily life can be replaced by vegetable oil, 60 grams a day or so. 3, in order to reduce the burden of kidney, foods containing high purine and high nitrogen should limit the foods that stimulate the kidneys, such as spinach, celery, radish, beans, soy products, sardine, chicken broth, fish soup, broth, etc. Because of the high purine and nitrogen content in those foods, when the renal function is poor, its metabolites can not be excreted in time, which has a negative impact on the renal function. 4. Strong condiment. Strong condiment is not good for kidney function and should be avoided. Monosodium glutamate will be thirsty after eating more. When limiting the amount of drinking water, we should also use less monosodium glutamate.