Prostatitis symptoms?
summary
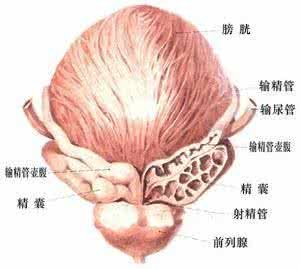
Prostatitis is caused by a variety of complex reasons, with urethral irritation symptoms and chronic pelvic pain as the main clinical manifestations of prostate disease. Prostatitis is a common disease in urology department, which is the first in male patients under 50 years old. Although the incidence rate of prostatitis is very high, the etiology is still not very clear, especially the non bacterial prostatitis, so its treatment is mainly to improve symptoms. Prostatitis symptoms? Let's talk about it
Prostatitis symptoms?
Type I prostatitis is often characterized by sudden onset of chills, fever, fatigue and weakness. It has perineal and suprapubic pain. It can cause frequent urination, * urgency and irritation of rectum, and even acute urinary retention.
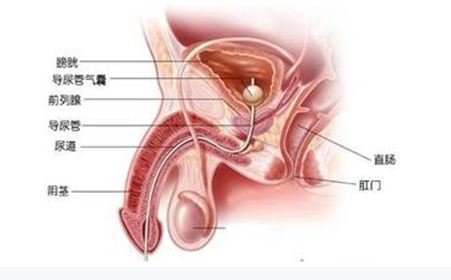
The clinical symptoms of type II and type III prostatitis are similar, with pain and abnormal urination. No matter which type of chronic prostatitis can show similar clinical symptoms, collectively known as prostatitis syndrome, including pelvic and sacral pain, dysuria and sexual dysfunction. The manifestation of pelvic sacral pain is extremely complex. The pain is generally located in the suprapubic, lumbosacral and perineal parts. Radiative pain can be manifested as pain in the urethra, spermatic cord, testis, inguinal and ventral side. Radiating to the abdomen is similar to acute abdomen, and radiating along the urinary tract is similar to renal colic, which often leads to misdiagnosis.
Abnormal urination is manifested as frequent urination, urgency, pain, poor urination, bifurcated urine line, dripping after urination, increased frequency of nocturia, and milky white secretion from urethra after urination or defecation. Occasionally complicated with sexual dysfunction, including loss of libido, premature ejaculation, ejaculation pain, erectile dysfunction and impotence.
matters needing attention
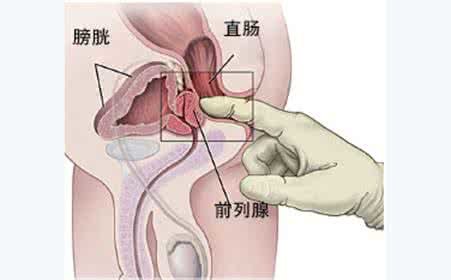
The pathogenic pathogens found in prostatic fluid culture are the basis for the selection of antimicrobial therapy. If there are signs of bacterial infection in patients with non bacterial prostatitis, the general treatment is ineffective, antibiotics can also be used appropriately. The selection of antimicrobial agents should pay attention to the existence of prostate blood barrier composed of lipid membrane between prostate acinus and microcirculation, which prevents the passage of water-soluble antibiotics and greatly reduces the therapeutic effect. When there are prostate stones, the stones can become a shield for bacteria. The above factors constitute the difficulty in the treatment of chronic bacterial prostatitis, which requires a long course of treatment and is easy to relapse.














