How to treat pulmonary embolism in the elderly?
summary
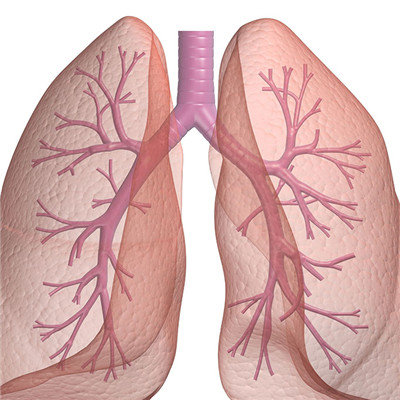
How to treat pulmonary embolism in the elderly? Pulmonary embolism (PE) is a pathological and clinical syndrome caused by blocking the blood supply of lung tissue by impaction material entering the pulmonary artery and its branches. The common embolus is thrombus, and the rare embolus is new biological cell mass, fat droplet, bubble and so on. Because of the dual blood supply of pulmonary artery and bronchial artery in lung tissue, and the direct gas exchange between lung tissue and alveolar gas, most pulmonary embolism may not form infarction, and there is no obvious clinical manifestation. Pulmonary embolism is a common disease in the elderly.
How to treat pulmonary embolism in the elderly?
General treatment of bed rest; Oxygen inhalation, if necessary, high frequency injection or oscillating oxygen supply; It is very important to keep defecation smooth and avoid the massive falling off of peripheral embolus. Symptomatic treatment maintained hemodynamic stability, timely corrected shock and heart failure, and given low molecular dextran to expand volume and improve hemorheology; Patients with severe chest pain were given analgesics; Cyproheptadine and ketoserine can effectively relieve vasospasm and airway spasm caused by embolization.
Thrombolytic therapy for pulmonary embolism or deep venous thrombosis is still controversial. However, for massive pulmonary embolism (embolizing more than two lobes) within 5 days or pulmonary embolism with hypotension, thrombolytic therapy is still recommended for those without contraindications. Urokinase is commonly used in China. The first dose is 2000-4400u / kg, which is injected intravenously within 10-30min, followed by 2000-4000u / kg per hour for 12-24h, followed by anticoagulant therapy. Another commonly used drug is alteplase (recombinant tissue plasminogen activator, RT PA). It selectively dissolves fibrin in the formed thrombus. Theoretically, it only has local thrombolytic effect and does not cause systemic thrombolytic effect. The dosage is 40-100mg, intravenous drip for more than 2 hours, and heparin is added.

Anticoagulant therapy can not directly dissolve the thrombus, but it can prevent the further development of thrombosis. Some patients with mild disease only use anticoagulant therapy, and can also obtain satisfactory curative effect through the body's own fibrinolysis process. Commonly used drugs are heparin and warfarin. Heparin is generally used in the initial stage of anticoagulation and after thrombolysis. It can prevent thrombosis and blood clot dissemination. The dosage is 15000-30000 U / D, and the coagulation time is controlled at 1.5-2 times of normal. Heparin is injected intravenously or subcutaneously, and adjusted according to the results of coagulation monitoring. Warfarin was added to heparin for 7-10 days, and warfarin was taken orally for 3-5 days. Studies have shown that low molecular weight heparin has the same effect as conventional heparin, but the bleeding complications are less. Warfarin is mainly used for maintenance treatment. The first dose of warfarin is 10-15mg, which is halved the next day, and then maintained at 2.5-7.5mg every day. The specific amount of warfarin is adjusted according to the condition of blood coagulation. In the past, prothrombin was required to be controlled to 1.5-2.5 times of the control value. Recently, warfarin maintenance treatment dose is recommended to control prothrombin at 1.3-1.6 times of the control value. The course of warfarin treatment is generally 3-6 months. Natural and recombinant hirudin (rhhirudin) can prevent thrombosis and has a good application prospect in the prevention and treatment of thrombosis and pulmonary embolism, which is still under further study.
matters needing attention
In view of the fact that the majority of pulmonary embolism comes from the thrombosis of deep vein or right heart cavity of lower limbs, the key to prevent pulmonary embolism is to prevent vascular endothelial injury, correct hypercoagulability and hyperviscosity, and prevent hemodynamic disorders (such as blood stasis and atrial fibrillation), Active treatment of varicose veins; ② Long term bedridden people should avoid pillow under popliteal fossa, encourage active activities and coughing of lower limbs in bed, wear long elastic socks or use inflatable boots to compress lower limbs intermittently, and encourage early out of bed activities.